History
The patient history is notable for exposure to the virus. The incubation period from exposure to onset of measles symptoms ranges from 7 to 14 days (average, 10-12 days). Patients are contagious from 1-2 days before the onset of symptoms. Healthy children are also contagious during the period from 3-5 days before the appearance of the rash to 4 days after the onset of rash. On the other hand, immunocompromised individuals can be contagious during the duration of the illness.
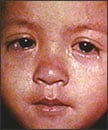
The first sign of measles is usually a high fever (often >104o F [40o C]) that typically lasts 4-7 days. This prodromal phase is marked by malaise, fever, anorexia, and the classic triad of conjunctivitis (see the image below), cough, and coryza (the “3 Cs”). Other possible associated symptoms include photophobia, periorbital edema, and myalgias.
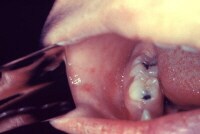
Measles conjunctivitis The characteristic enanthem generally appears 2-4 days after the onset of the prodrome and lasts 3-5 days. Small spots (Koplik spots) can be seen inside the cheeks during this early stage (see the image below).
Koplik spots in measles. Photograph courtesy of World Health Organization. The exanthem usually appears 1-2 days after the appearance of Koplik spots; mild pruritus may be associated. On average, the rash develops about 14 days after exposure, starting on the face and upper neck (see the image below) and spreading to the extremities. Immunocompromised patients may not develop a rash.
Child with measles. Photograph courtesy of Centers for Disease Control and Prevention. The entire course of uncomplicated measles, from late prodrome to resolution of fever and rash, is 7-10 days. Cough may be the final symptom to appear.
Atypical measles occurs in individuals who were vaccinated with the original killed-virus measles vaccine between 1963 and 1967 and who have incomplete immunity. After exposure to the measles virus, a mild or subclinical prodrome of fever, headache, abdominal pain, and myalgias precedes a rash that begins on the hands and feet and spreads centripetally. The eruption is accentuated in the skin folds and may be macular, vesicular, petechial, or urticarial. The live-attenuated vaccine replaced the killed vaccine in 1967 and is not associated with atypical measles.
Enanthem of measles (Koplik spots) The Koplik spots generally are first seen 1-2 days before the appearance of the rash and last until 2 days after the rash appears. This enanthem begins to slough as the rash appears. Although this is the pathognomonic enanthem of measles, its absence does not exclude the diagnosis.
 Face of boy with measles
Face of boy with measles  Morbilliform rash Patients appear most ill during the first or second day of the rash. The exanthem lasts for 5-7 days before fading into coppery brown hyperpigmented patches, which then desquamate. The rash may be absent in patients with underlying deficiencies in cellular immunity.
Morbilliform rash Patients appear most ill during the first or second day of the rash. The exanthem lasts for 5-7 days before fading into coppery brown hyperpigmented patches, which then desquamate. The rash may be absent in patients with underlying deficiencies in cellular immunity.

Complications of measles are more likely to occur in persons younger than 5 years or older than 20 years, and complication rates are increased in persons with immune deficiency disorders, malnutrition, vitamin A deficiency, and inadequate vaccination. Immunocompromised children and adults are at increased risk for severe infections and superinfections.
Common infectious complications include otitis media, interstitial pneumonitis,[19] bronchopneumonia, laryngotracheobronchitis (ie, croup), exacerbation of tuberculosis, transient loss of hypersensitivity reaction to tuberculin skin test, encephalomyelitis, diarrhea, sinusitis, stomatitis, subclinical hepatitis, lymphadenitis, and keratitis, which can lead to blindness. In fact, measles remains a common cause of blindness in many developing countries.
Rare complications include hemorrhagic measles, purpura fulminans, hepatitis, disseminated intravascular coagulation (DIC), subacute sclerosing panencephalitis (SSPE), thrombocytopenia, appendicitis, ileocolitis, pericarditis, myocarditis, acute pancreatitis,[20] and hypocalcemia.[21] Transient hepatitis may occur during an acute infection.
Approximately 1 of every 1,000 patients develops acute encephalitis, which often results in permanent brain damage and is fatal in about 10% of patients. In children with lymphoid malignant diseases, delayed-acute measles encephalitis may develop 1-6 months after the acute infection and is generally fatal.
An even rarer complication is SSPE, a degenerative CNS disease that can result from a persistent measles infection. SSPE is characterized by the onset of behavioral and intellectual deterioration and seizures years after an acute infection (the mean incubation period for SSPE is approximately 10.8 years).
The complications of measles in the pregnant mother include pneumonitis, hepatitis, subacute sclerosing panencephalitis, premature labor, spontaneous abortion, and preterm birth of the fetus. Perinatal transmission rates are low
The first sign of measles is usually a high fever (often >104o F [40o C]) that typically lasts 4-7 days. This prodromal phase is marked by malaise, fever, anorexia, and the classic triad of conjunctivitis (see the image below), cough, and coryza (the “3 Cs”). Other possible associated symptoms include photophobia, periorbital edema, and myalgias.
Gift for your baby...
Measles conjunctivitis The characteristic enanthem generally appears 2-4 days after the onset of the prodrome and lasts 3-5 days. Small spots (Koplik spots) can be seen inside the cheeks during this early stage (see the image below).
Koplik spots in measles. Photograph courtesy of World Health Organization. The exanthem usually appears 1-2 days after the appearance of Koplik spots; mild pruritus may be associated. On average, the rash develops about 14 days after exposure, starting on the face and upper neck (see the image below) and spreading to the extremities. Immunocompromised patients may not develop a rash.
Child with measles. Photograph courtesy of Centers for Disease Control and Prevention. The entire course of uncomplicated measles, from late prodrome to resolution of fever and rash, is 7-10 days. Cough may be the final symptom to appear.
Modified and atypical measles
Modified measles is a milder form of measles that occurs in individuals who have received serum immunoglobulin after their exposure to the measles virus. Similar but milder symptoms and signs may still occur, but the incubation period may be as long as 21 days.Atypical measles occurs in individuals who were vaccinated with the original killed-virus measles vaccine between 1963 and 1967 and who have incomplete immunity. After exposure to the measles virus, a mild or subclinical prodrome of fever, headache, abdominal pain, and myalgias precedes a rash that begins on the hands and feet and spreads centripetally. The eruption is accentuated in the skin folds and may be macular, vesicular, petechial, or urticarial. The live-attenuated vaccine replaced the killed vaccine in 1967 and is not associated with atypical measles.
Physical Examination
Enanthem
Near the end of the prodrome, Koplik spots (ie, bluish-gray specks or “grains of sand” on a red base) appear on the buccal mucosa opposite the second molars (see the image below).
Enanthem of measles (Koplik spots) The Koplik spots generally are first seen 1-2 days before the appearance of the rash and last until 2 days after the rash appears. This enanthem begins to slough as the rash appears. Although this is the pathognomonic enanthem of measles, its absence does not exclude the diagnosis.
Exanthem
Blanching, erythematous macules and papules begin on the face at the hairline, on the sides of the neck, and behind the ears (see the images below). Within 48 hours, they coalesce into patches and plaques that spread cephalocaudally to the trunk and extremities, including the palms and soles, while beginning to regress cephalocaudally, starting from the head and neck. Lesion density is greatest above the shoulders, where macular lesions may coalesce. The eruption may also be petechial or ecchymotic in nature. Face of boy with measles
Face of boy with measles  Morbilliform rash Patients appear most ill during the first or second day of the rash. The exanthem lasts for 5-7 days before fading into coppery brown hyperpigmented patches, which then desquamate. The rash may be absent in patients with underlying deficiencies in cellular immunity.
Morbilliform rash Patients appear most ill during the first or second day of the rash. The exanthem lasts for 5-7 days before fading into coppery brown hyperpigmented patches, which then desquamate. The rash may be absent in patients with underlying deficiencies in cellular immunity.
Complications
Most complications of measles occur because the measles virus suppresses the host’s immune responses, resulting in a reactivation of latent infections or superinfection by a bacterial pathogen. Consequently, pneumonia, whether due to the measles virus itself, to tuberculosis, to or another bacterial etiology, is the most frequent complication. Pleural effusion, hilar lymphadenopathy, hepatosplenomegaly, hyperesthesia, and paresthesia may also be noted.Common infectious complications include otitis media, interstitial pneumonitis,[19] bronchopneumonia, laryngotracheobronchitis (ie, croup), exacerbation of tuberculosis, transient loss of hypersensitivity reaction to tuberculin skin test, encephalomyelitis, diarrhea, sinusitis, stomatitis, subclinical hepatitis, lymphadenitis, and keratitis, which can lead to blindness. In fact, measles remains a common cause of blindness in many developing countries.
Rare complications include hemorrhagic measles, purpura fulminans, hepatitis, disseminated intravascular coagulation (DIC), subacute sclerosing panencephalitis (SSPE), thrombocytopenia, appendicitis, ileocolitis, pericarditis, myocarditis, acute pancreatitis,[20] and hypocalcemia.[21] Transient hepatitis may occur during an acute infection.
Approximately 1 of every 1,000 patients develops acute encephalitis, which often results in permanent brain damage and is fatal in about 10% of patients. In children with lymphoid malignant diseases, delayed-acute measles encephalitis may develop 1-6 months after the acute infection and is generally fatal.
An even rarer complication is SSPE, a degenerative CNS disease that can result from a persistent measles infection. SSPE is characterized by the onset of behavioral and intellectual deterioration and seizures years after an acute infection (the mean incubation period for SSPE is approximately 10.8 years).
The complications of measles in the pregnant mother include pneumonitis, hepatitis, subacute sclerosing panencephalitis, premature labor, spontaneous abortion, and preterm birth of the fetus. Perinatal transmission rates are low
References
- Sabella C. Measles: not just a childhood rash. Cleve Clin J Med. Mar 2010;77(3):207-13. [Medline].
- [Guideline] Centers for Disease Control and Prevention. Recommended immunization schedules for persons aged 0 through 18 years---United States, 2009. CDC Recommended Vaccine Schedule. Dec 2008;57(51;52):[Full Text].
- Meissner HC, Strebel PM, Orenstein WA. Measles vaccines and the potential for worldwide eradication of measles. Pediatrics. 2004;114(4):1065-9. [Medline]. [Full Text].
- Smeeth L, Cook C, Fombonne E, et al. MMR vaccination and pervasive developmental disorders: a case-control study. Lancet. 2004;11-17;364(9438):963-9. [Medline].
- Schneider-Schaulies S, Schneider-Schaulies J. Measles virus-induced immunosuppression. Curr Top Microbiol Immunol. 2009;330:243-69. [Medline].
- Markowitz LE, Preblud SR, Fine PE, Orenstein WA. Duration of live measles vaccine-induced immunity. Pediatr Infect Dis J. Feb 1990;9(2):101-10. [Medline].
- Reported vaccine-preventable diseases--United States, 1993, and the childhood immunization initiative. MMWR Morb Mortal Wkly Rep. Feb 4 1994;43(4):57-60. [Medline].
- Orenstein WA, Papania MJ, Wharton ME. Measles elimination in the United States. J Infect Dis. May 1 2004;189 Suppl 1:S1-3. [Medline].
- Coleman KP, Markey PG. Measles transmission in immunized and partially immunized air travellers. Epidemiol Infect. Jul 2010;138(7):1012-5. [Medline].


 Subscribe to email feed
Subscribe to email feed



